Iatrogenic Resuscitation
Current Resuscitation Practice
When any “at risk” child is delivered, the cord is clamped and cut immediately and prompt airway clearing and ventilation are done on a warmer. This is not revival; it is rapid, forced removal from placental life support to hasty pulmonary respiration. It results in major disruptions of perinatal physiology and neonatal life support systems.
When a child is born depressed,
“asphyxiated”, atonic and unable to breathe, the pathology is not due to cardiac
or pulmonary failure, the defect is in the placenta and / or umbilical cord;
the most common cause is intra-partum cord compression.
If
the cord is still pulsating, failure is not total – the cord is maintaining
life, and placental / cord function should be restored, not amputated, in order
to maximize revival of the child. This
principle is used successfully to correct fetal distress in utero – changing
maternal position to relieve cord compression. Iatrogenic resuscitation (IR)
discards this advantage.
IR
disrupts much of the anatomy and physiology involved in the normal transition
from placental to independent life support:
·
Immediate cord clamping
terminates placental respiration, imposing complete asphyxia on the neonate
’til pulmonary function is established.
·
Immediate cord clamping
prevents placental transfusion, a loss of up to 50+% of the neonate’s blood
volume, resulting in:
1.
Drastic reduction in
venous return to the heart and reduction in cardiac output – see the
precipitous fall in the heart rate at cord clamping in [A].
2.
Loss of the “jaykka”
effect in expanding alveoli.
3.
Diminished pulmonary
perfusion and possible non-closure of the foramen ovale – persistent fetal
circulation.
4.
Diminished perfusion of
all neonatal life support systems – heart, lungs, brain, kidneys, gut and
respiratory muscles.
·
The warmer deprives the
child of the “cold crying” and “cold pressor” reflexes.
·
Ventilation relaxes
pulmonary arterioles, but diverting blood volume into the lung vessels may
collapse the systemic circulation – hypovolemic shock.
The
effects of immediate clamping (hypovolemia) are apparent on many newborns:
i.
Pallor, lethargy,
weakness
ii.
Hypoglycemia: liver
ischemia reduces production of glucose.
iii.
Hypotension.
iv.
Kidney failure/low
urine output.
v.
Severe anemia and blood
transfusion.
vi.
Hypovolemic neonates
may become hypothermic.
vii.
The “shock lung
syndrome” [RDS] and hyaline membrane disease.
viii.
Retraction respiration,
ischemic encephalopathy and brain damage.
All
these complications may be avoided by resuscitating the depressed neonate with
the placental circulation intact and by allowing the umbilical vessels to close
physiologically, permitting full placental transfusion.
Note:
If a neonate is born limp, ashen pale, without
reflexes, meconium stained, a cord pulse rate of 60 b.p.m. and a firm, true
knot in the cord, would you:
1.
Clamp the cord
immediately to obtain a cord pH?
2.
Or would you loosen the
knot?
www.cordclamping.com Neonatal Resuscitation: Life that Failed.
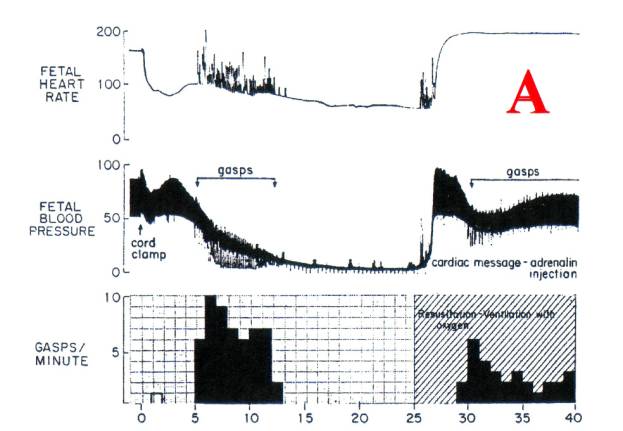
Figure 1. Myers
RE. Perinatal brain damage. American Journal of Obstetrics and
Gynecology 1972 112:246-276.30
Copyright September 2004 G. M. Morley MB ChB FACOG